BURDEN OF DISEASE
Acute rheumatic fever and rheumatic heart disease were once common across the world, including in Australia, Europe, Great Britain, and North America. Rates of disease declined in many countries during the mid-20th century, and this was associated with improvements in housing and socioeconomic conditions, better access to healthcare, and increasing availability of penicillin to treat streptococcal (Strep A) infections.
In Australia, rheumatic fever and rheumatic heart disease continue to cause significant ill-health and premature death at high rates primarily among First Nations communities. The burden of disease often spans the majority of a person’s lifetime, starting with ARF in childhood, and progressing in many cases to rheumatic heart disease and its complications during adulthood.
Many high-income countries, including Australia, have a residual burden of rheumatic heart disease among older surviving adults who developed rheumatic fever in their youth prior to improvements in socioeconomic conditions and antibiotic treatment. In Australia, disease registers are used to help coordinate care for people with rheumatic fever and rheumatic heart disease.
CULTURE AT THE CENTRE OF CARE
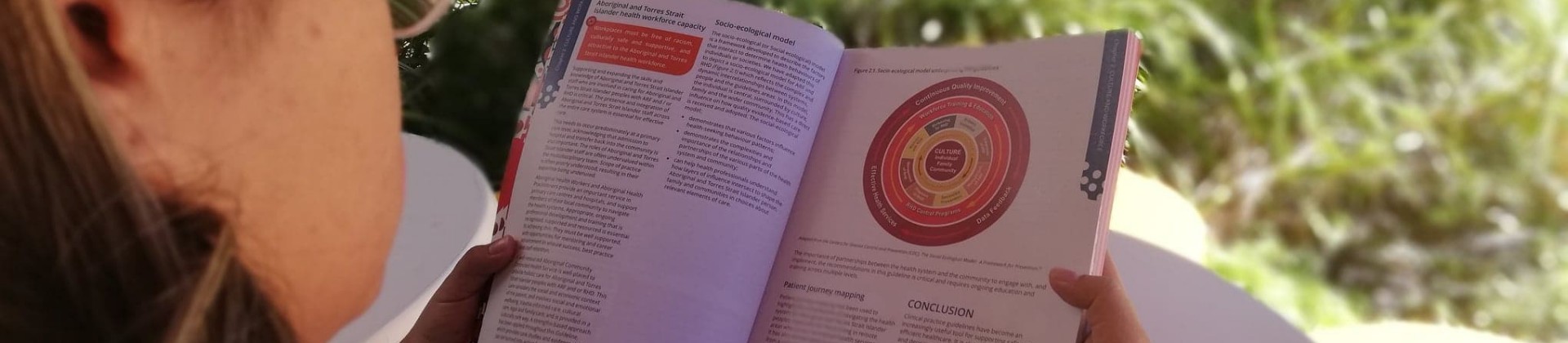
Many cultures across the world have a holistic view of health that does not necessarily align with the western biomedical model of healthcare. Health is not just the physical wellbeing of an individual, but refers to the social, emotional, and cultural wellbeing of the whole community.
In Australia, effective and comprehensive healthcare delivery that is culturally safe, responsive and adaptable to local contexts and cultural diversity – particularly First Nations communities – is necessary to close the evidence-practice gap.
PRIMORDIAL PREVENTION
Primordial disease prevention addresses the root causes of disease. For rheumatic fever, this means addressing the causes of high rates of Strep A infections in a community, which include addressing safe housing and environments, adequate sanitation and washing facilities, and timely healthcare.
PRIMARY PREVENTION OF RHEUMATIC FEVER
Rheumatic fever results from an abnormal immune system response to a Strep A infection. Primary prevention of rheumatic fever aims to interrupt immune system priming in response to Strep A infections of the throat and skin.
In Australia, people at high risk and low risk of rheumatic fever are managed differently. Currently (in the absence of widely available, accurate point-of-care Strep A tests), everyone who is at high risk of rheumatic fever should be offered antibiotic treatment for sore throat and skin sores, due to the higher risk of rheumatic fever and rheumatic heart disease if a Strep A infection is missed. Recommended treatment is either one intramuscular long acting benzathine benzylpenicillin injection or a course of antibiotic tablets or syrup. People at low risk should be offered treatment if investigation confirms Strep A infection.
DIAGNOSIS AND MANAGEMENT OF RHEUMATIC FEVER
Rheumatic fever is a self-limiting, inflammatory illness that can affect the joints, skin, heart and/or brain. Involvement of the heart during rheumatic fever is called carditis. There is no single diagnostic test available. Correct diagnosis requires the use of a specific diagnostic algorithm incorporating clinical assessment and investigation of the presenting symptoms and signs. Strep A infections and rheumatic fever are most common in children and adolescents. Severity of symptoms range from very mild, to severe where the person may be bed-bound due to joint pain, heart failure or movement disorder (chorea). Rheumatic fever does not present the same way for everyone, and symptoms rarely all occur at the same time.
Medical management is based on confirming the diagnosis, treating the Strep A infection, and determining whether the heart is involved using an echocardiogram (ultrasound of the heart). Hospital care is highly recommended and includes close monitoring, symptom management, culturally appropriate education, and developing a plan for longer-term care including secondary prophylaxis where required and follow up echocardiograms.
A smartphone Application is available to support clinicians with rheumatic fever diagnosis and management in the Australian context.
DIAGNOSIS AND MANAGEMENT OF RHEUMATIC HEART DISEASE
Rheumatic heart disease is damage to the structure and function of one or more heart valves. It can be mild, moderate or severe. Many people have mild disease with no symptoms. This may be detectable as a heart murmur which can be heard through a stethoscope but is best evaluated with an echocardiogram (ultrasound). Rheumatic heart disease develops following one or more episodes of rheumatic fever with carditis. The valves become stiff and scarred; they do not open properly or do not close properly. This interrupts normal blood flow through the heart, but symptoms may not be noticed for many years. Many people can live a normal life expectancy with well-managed rheumatic heart disease. However, complications of rheumatic heart disease cause progressive disability, reduce quality of life, and can lead to premature death.
Medical management focuses on relieving symptoms and supporting heart function to prevent or reduce the impact of complications. Heart valve surgery is needed for people with severe disease to improve blood flow, manage symptoms and improve length and quality of life.
SECONDARY PREVENTION OF RHEUMATIC FEVER
Children and young adults living with rheumatic fever and rheumatic heart disease usually require regular, long-term antibiotic prophylaxis to prevent further Strep A infections and recurrent rheumatic fever. Antibiotics are most effectively delivered as intramuscular benzathine benzylpenicillin injections every 21 to 28 days during the period of highest risk, which for most people continues into young adulthood. Tablet alternatives are available for people with a documented penicillin allergy, although this may be less effective in preventing rheumatic fever and requires careful monitoring. The duration of antibiotic prophylaxis depends on several factors including age at diagnosis, recurrent rheumatic fever illnesses, severity of rheumatic heart disease if it is present, and the ongoing risk of further Strep A infections. An echocardiogram and medical specialist review are required before secondary prevention treatment can be ceased.
Receiving and providing injections and other medical care over many years can be difficult for patients, families and health services. Health services can support people who experience difficulties with injections by providing competent and patient-centred care and using strategies to minimise injection pain and distress.
SCREENING FOR RHEUMATIC HEART DISEASE
Echocardiographic screening to detect early stage rheumatic heart disease in high-risk populations has been widely used in Australia and internationally, both in research settings to estimate the burden of disease, and as part of community-led programs. Screening procedures have evolved over time, using different technologies and involving operators with varying levels of expertise.
There have been significant advances in ultrasound technology, including the development of small portable echocardiogram devices and handheld machines. Smaller portable devices make screening more accessible in remote areas. Research has also involved training non-expert operators to obtain the limited echocardiographic images required to detect RHD.
To support screening and ongoing monitoring of rheumatic heart disease, the World Heart Federation has published international guidelines for diagnosis and staging of rheumatic heart disease using echocardiography.
WOMEN AND GIRLS WITH RHEUMATIC HEART DISEASE
Rheumatic heart disease is twice as common in women as in men. In Australia, First Nations women, Māori and other Pacific Islander women, and women from other countries with high rates of disease are at higher risk for rheumatic heart disease. Medical and social care includes managing rheumatic fever and rheumatic heart disease within the context of reproductive health. Preparing for potential heart valve surgery and timing of pregnancies should start early for young women who are diagnosed with rheumatic fever and rheumatic heart disease.
More information is available in the Australian guideline for the prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease (3rd edition).